A SOAP Note Template is an essential tool used by therapists, counselors, and healthcare professionals to document client sessions effectively.
This structured format ensures clear and concise record-keeping, making it easier to track a client’s progress over time.
Unlike many other websites that charge for such templates, this Simple Therapy Note is available for free and can be edited directly in Google Docs.
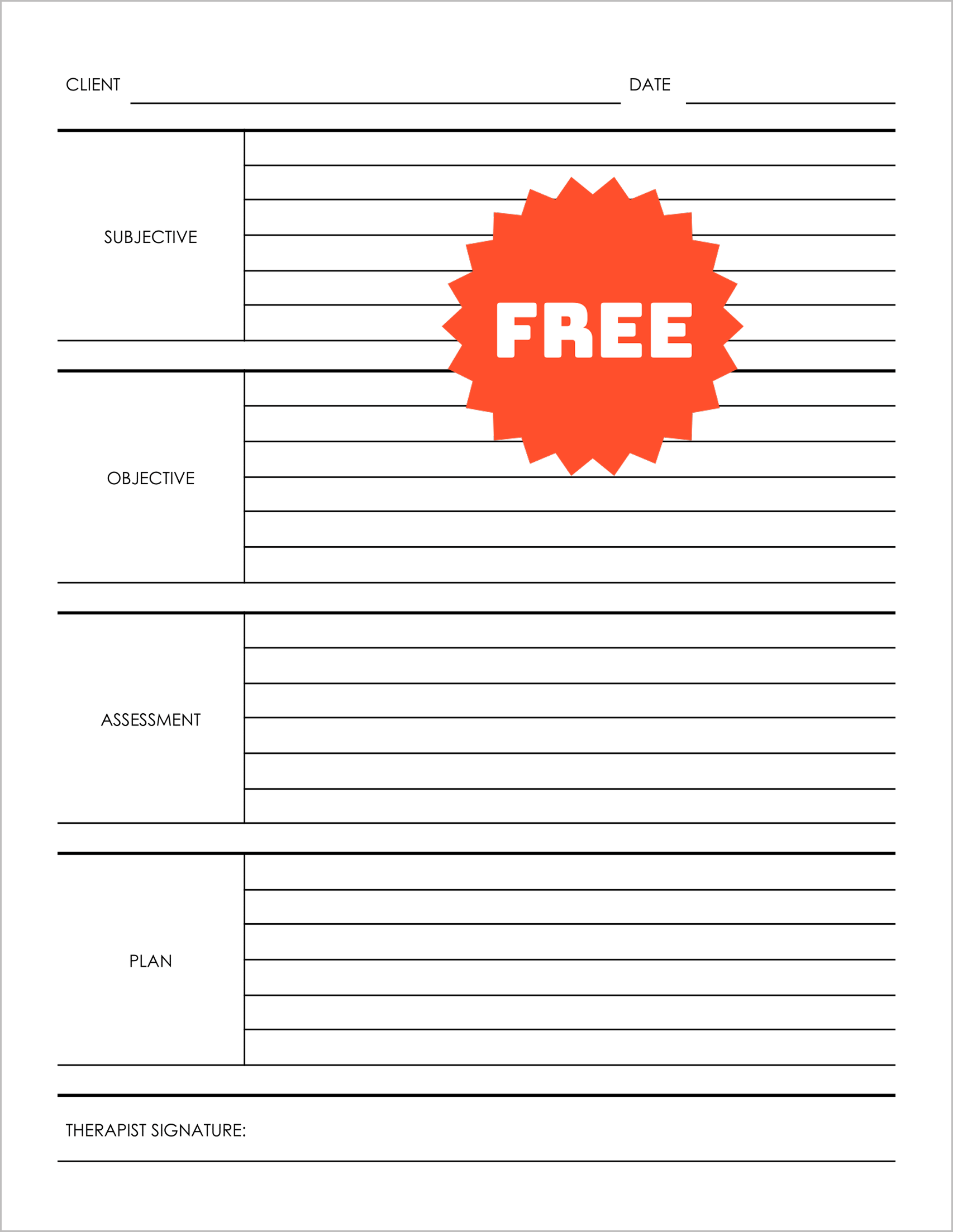
What is a SOAP Note?
SOAP notes follow a standardized format used in various healthcare and therapy settings.
The acronym stands for:
- Subjective – The client’s self-reported condition, feelings, or symptoms.
- Objective – The therapist’s observations, assessments, or test results.
- Assessment – The therapist’s professional evaluation based on the subjective and objective data.
- Plan – The proposed treatment plan, next steps, or follow-ups.
This Counselor Note format ensures that all necessary information is documented in an organized manner, improving communication between healthcare professionals and ensuring better client care.
Why Use This Free SOAP Note Template?
- Easy to Edit & Customize – This template is available in Google Docs, allowing instant access and customization without requiring any software installation.
- Professional & Standardized Format – Ideal for counselors, therapists, and medical professionals who need a structured Progress Note format.
- Free to Use – Unlike other paid options, this template is completely free and ready for immediate use.
Template Fields
CLIENT
DATE
SUBJECTIVE
OBJECTIVE
ASSESSMENT
PLAN
THERAPIST SIGNATURE
Free Editable SOAP Note Template
- Click on the “Get this template” button.
- On the preview page, click “USE TEMPLATE” to make a copy.
- Start editing the fields as needed for your session notes.
- Save, print, or share the completed SOAP note.
This structured SOAP Note Template simplifies therapy documentation while maintaining professional standards. Start using it today for efficient and organized record-keeping.